TABLE OF CONTENT
- What Is the Mental Health Act 1983
- Key Sections of the Mental Health Act 1983
- Your Rights Under the Law: Mental Health Act 1983
- Why Mental Health Act 1983 Matters for Healthcare Staff
- Key Roles of Health Experts under the Mental Health Act 1983
- Mental Health Law for Healthcare Professionals Guide
- Other Legal Tools: The Mental Capacity Act 2005
- Guidelines from Professional Bodies
- How Mental Health Stigma Affects Lives
- Impact of Mental Health Stigma on Legal Outcomes
- Fighting Stigma: What Can Be Done
- The Role of Multidisciplinary Teams
- Let’s End the Stigma
- Get Legal and Clinical Mental Health Support
- FAQs
People’s health significantly depends on their mental condition which often remains unnoticed by health services. Mental health stigma impedes the proper delivery of care for treating mental health conditions throughout the UK. The Mental Health Act 1983 guarantees your rights and ensures your welfare is considered at every stage of your treatment.
“There can be no health without mental health. Mental health is a fundamental part of being human.”
Jemima Gordon-Duff, Speech at the British High Commission, Accra (14 Oct 2019)
Through Mental Health Act 1983 patients obtain support in treatment while caregivers receive assistance for their supportive role.
What Is the Mental Health Act 1983
The Mental Health Act 1983 shows how to assess and support people with serious mental health conditions. It also sets rules for authorities on when they can detain them. Mental Health Act 1983 allows medical experts to act when a person’s condition threatens their safety or the safety of others. It also establishes clear rules to guarantee that individuals exercise this power with fairness. It respects an individual’s rights of dignity.
This act lets health workers:
- Assess mental illness
- Give treatment
- Protect patient rights
Key Sections of the Mental Health Act 1983
Let’s analyse some fundamental features of the Mental Health Act 1983 and what they indicate.
Section 2 – Admission for Assessment
This allows someone to be kept in the hospital for up to 28 days for assessment.Key points of the section include:
- It is used when the person may have a mental disorder.
- The Doctors and an Approved Mental Health Professional must agree on the decision.
- The person has the right to appeal this decision.
Section 3 – Admission for Treatment
If a person also needs a treatment, after assessment, this section will be applied. According to this section:
- The person can stay for up to 6 months (can be renewed).
- The person must have a treatable mental condition.
- The goal is to protect both the person and others.
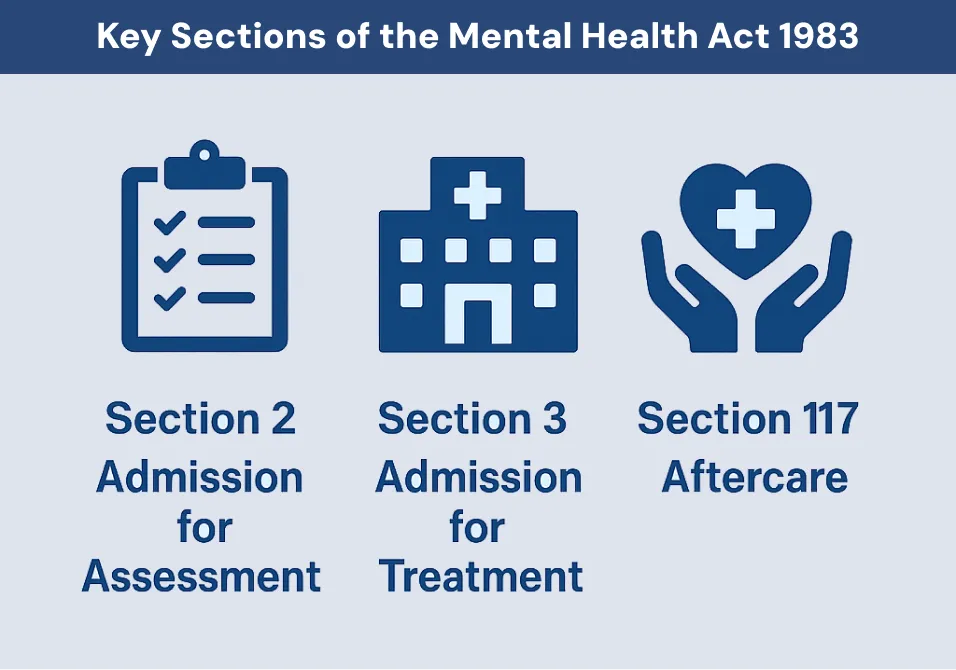
Section 117 – Aftercare
This section helps people after hospital discharge. Examples of supported services include:
- Providing free aftercare services.
- Covering therapy, medication, housing, or support.
- Getting it arranged by the NHS and social services.
These sections aim to support health while respecting personal rights.
The 1983 Mental Health Act is active in all hospitals as well as clinics and care homes.. It also has rules for aftercare and appeals.
Your Rights Under the Law: Mental Health Act 1983
If you or someone you know has mental illness, you have following rights under Mental Health Act 1983:
Right to fair care
Your treatment should be designed around your needs. Clear protocols ensure every patient receives fair and consistent support. This helps you feel safe and supported.
Right to be heard
You can share your views on your treatment plan and daily care. Your opinions must be taken seriously, and you can ask for a meeting if you feel ignored. Speaking up helps staff understand what works best for you.
Right to be free from abuse
You should never face harm, bullying, or neglect while in care. If you feel threatened, you can report it to a senior staff member or advocacy service. Keeping you safe is a legal duty for all professionals.

Right to appeal detention
If you are held under the Act, you can challenge that decision in a tribunal. You will be given information on how to apply and who can help you. This process lets you argue your case in front of an independent panel.
HL v UK Case
In HL v UK, a disabled man (HL) was informally held at a hospital without proper legal process. He could not leave and staff made decisions for him. He claimed under Article 5, and the European Court of Human Rights said his right to liberty was breached. This led to changes in the Mental Health Act to include formal safeguards for people who cannot consent to care. Added patient safety checks
Right to privacy and respect
Your personal information and treatment details must stay confidential. Staff knock and wait for your response before they come in. They speak politely and treat you with respect in every interaction to protect your privacy and dignity.
You can use these rights in schools, jobs, homes, and even courts.
Why Mental Health Act 1983 Matters for Healthcare Staff
The Act guarantees fair treatment for patients. It helps reduce stigma and mental health bias in healthcare and law. Patients can:
- Refuse treatment (in some cases), because when you have capacity, you can refuse treatment. Staff must explain the risks and alternatives so you can make an informed choice.
- You can appeal a detention decision through a tribunal if you believe it’s wrong.
- Get aftercare under Section 117. This may include therapy sessions, medication reviews, and help with housing or benefits.
In 2022–23, authorities detained over 51,312 people under this Mental Health Act 1983.
Key Roles of Health Experts under the Mental Health Act 1983
1. Sectioning
- If you’re in a mental health crisis that puts you or others at serious risk, doctors can admit you to hospital without your consent. Two different doctors must examine your situation and agree on the need for detention, each relying on clear medical evidence.
- Detention can cover a short period for assessment or longer for treatment, depending on what the person needs.
2. Patient Rights
If you’re brought into hospital under the Mental Health Act 1983, you do not lose your say in your own care. Staff should sit down with you in plain, everyday language to explain why you’re here and what the next steps will look like. You can speak to a solicitor and ask for an independent mental health advocate to support you. You also have the right to know how long your detention might last and what reviews will take place.
Legal Safeguards
People admitted under the Mental Health Act 1983 can request a review by a Mental Health Tribunal. Panel members study your medical notes and listen to your own account. If they find continued detention unnecessary, they’ll order your release. When the Tribunal grants release, the hospital arranges your discharge. Your social worker or chosen advocate can help you complete the application and prepare for the hearing.
3. Review and Care
A psychiatrist, a nurse and a social worker meet with you at regular intervals. In these meetings they check how you’re doing, update your treatment plan when your needs change and agree on what happens next. As you get better, they put in place follow-up support to help you return to everyday life safely.
Doctors must apply the Mental Health Act 1983 carefully, balancing safety and individual rights.
Mental Health Law for Healthcare Professionals Guide
Doctors, nurses, and mental health staff must know the law. They must give:
- Safe treatment
- Ethical treatment
- Lawful services
This is where the Mental Health Law for Healthcare Professionals Guide helps.
It teaches staff how to:
- Spot abuse
- Report harm
- Follow rules when a person lacks capacity
Staff who ignore these legal requirements could face court action.
Other Legal Tools: The Mental Capacity Act 2005
This Act steps in when someone can’t make their own treatment decisions. Under it, doctors assess a person’s ability to decide for themselves and, if they lack that capacity, make choices in the person’s best interest. In this way, it protects individuals with severe learning or mental impairments.
Read more details about What Is Testamentary Capacity.
Guidelines from Professional Bodies
Apart from the law, other UK groups also guide about treatment:
- GMC: General Medical Council
- NMC: Nursing and Midwifery Council
- HCPC: Health and Care Professions Council
Their rules help health staff act within the law and avoid mental health stigma.
How Mental Health Stigma Affects Lives
Mental health stigma and awareness are two sides of a coin. Stigma is the shame or blame placed on people with mental illness. This can be:
Public stigma
When people hear “mental illness” and think “weak” or “dangerous,” it can shut down any chance of asking for help. Rumors, teasing, or being left out often follow. That isolation makes it even harder to reach out.
Self-stigma
Blaming yourself for your struggles brings shame. You may hide your feelings and skip appointments. Over time, avoiding support only makes recovery tougher.
Legal or institutional bias
Some laws and policies assume mental health issues mean someone can’t be trusted. That bias shows up in child custody cases, court sentences, or when services are denied.
This leads to:
Less care access
Worries about being judged keep many from seeking help. Delayed treatment allows symptoms to grow and become more challenging.
Poor job chances
Employers might doubt a person’s reliability or skills. This can block promotions or even cost them their job.
Bias in legal outcomes
Sometimes a quivering voice or trouble focusing is read as lying or aggression by police or judges. Because of this, someone might get stricter bail conditions, a longer sentence, or lose access to support. A UK Parliament study found people with mental health problems die 15 to 25 years earlier on average than others. It underscores the real cost of these errors.
Impact of Mental Health Stigma on Legal Outcomes
Bias in courts and law can be deadly. People with mental health issues may face:
- Unfair treatment in custody cases, such as Judges viewing them as unstable and removing their children from their care.
- Jurors doubt their testimony, doubting what happened, who was involved, or key details of the incident, assuming confusion.
- Mistaken use of force during arrest for instance police officers mistaking a panic attack for aggression and using excessive force.
Judges, police, and juries may hold hidden biases. This affects the legal outcome even when the law is on the patient’s side.
Fighting Stigma: What Can Be Done
The UK has launched campaigns with charities to challenge misconceptions and reduce mental health stigma by spreading awareness. However, significant gaps remain that demand further action. Here are steps that can help:
Education
- Teach kids about mental health in school.
- Train doctors, teachers, and lawyers on empathy and rights.
- Add courses on mental health stigma and awareness.
Policy Reform
- Review laws to protect against bias
- Improve access to mental health services
- Fund public awareness drives
Community Support
- Promote open talks at work, school, and home
- Help people share their stories
- Challenge the media that spreads false ideas
Better Healthcare Practices
- Train staff on Mental Health Law for Healthcare Professionals Guide.
- Hold team meetings to discuss patient care.
- Make care plans that match the law and patient needs.
The Role of Multidisciplinary Teams
Treatment in the UK is team-based. A care team may include:
- Psychiatrists
They are medical doctors who diagnose mental health conditions and map out your treatment. They may prescribe medications, suggest therapies, and do regular checkups to see your recovery.
- Nurses
Staff check vital signs, administer pills, and watch how patients respond day to day. They deliver your medications on schedule and note how you respond. Any changes get passed along to your doctor right away.
- Social workers
They help you sort out practical needs like housing or benefits applications. They will walk you through any paperwork and help set up that first meeting or call.
- Therapists
Experts provide face to face counseling or group sessions to help patients work through thoughts and feelings.
Each person has a legal role. They must:
- Share updates by sending reports or speaking at team meetings so everyone knows the patient’s progress.
- Review treatment in regular case reviews to decide if medications or therapies need changing.
- Record notes immediately after every contact to keep a clear, lawful record of what happened.
This keeps care safe, fair, and within the law.
Let’s End the Stigma
The Mental Health Act 1983 and other UK laws protect your mental well-being. But we must also fight mental health stigma. This means:
- Knowing your rights
- Getting fair treatment
- Helping others understand
Change begins with awareness. And support begins with care.
Get Legal and Clinical Mental Health Support
Concise Medico provides expert psychiatry witness reports, mental health assessments, and legal-medical opinions aligned with the Mental Health Act 1983. Our team makes sure evaluations follow UK laws. We also promote patient dignity and work to reduce mental health stigma.
Contact Us to learn more or book a consultation.
FAQs
People’s health significantly depends on their mental condition which often remains unnoticed by health services. Mental health stigma impedes the proper delivery of care for treating mental health conditions throughout the UK. The Mental Health Act 1983 guarantees your rights and ensures your welfare is considered at every stage of your treatment.
“There can be no health without mental health. Mental health is a fundamental part of being human.”
Jemima Gordon-Duff, Speech at the British High Commission, Accra (14 Oct 2019)
Through Mental Health Act 1983 patients obtain support in treatment while caregivers receive assistance for their supportive role.
What Is the Mental Health Act 1983
The Mental Health Act 1983 shows how to assess and support people with serious mental health conditions. It also sets rules for authorities on when they can detain them. Mental Health Act 1983 allows medical experts to act when a person’s condition threatens their safety or the safety of others. It also establishes clear rules to guarantee that individuals exercise this power with fairness. It respects an individual’s rights of dignity.
This act lets health workers:
- Assess mental illness
- Give treatment
- Protect patient rights
Key Sections of the Mental Health Act 1983
Let’s analyse some fundamental features of the Mental Health Act 1983 and what they indicate.
Section 2 – Admission for Assessment
This allows someone to be kept in the hospital for up to 28 days for assessment.Key points of the section include:
- It is used when the person may have a mental disorder.
- The Doctors and an Approved Mental Health Professional must agree on the decision.
- The person has the right to appeal this decision.
Section 3 – Admission for Treatment
If a person also needs a treatment, after assessment, this section will be applied. According to this section:
- The person can stay for up to 6 months (can be renewed).
- The person must have a treatable mental condition.
- The goal is to protect both the person and others.
Section 117 – Aftercare
This section helps people after hospital discharge. Examples of supported services include:
- Providing free aftercare services.
- Covering therapy, medication, housing, or support.
- Getting it arranged by the NHS and social services.
These sections aim to support health while respecting personal rights.
The 1983 Mental Health Act is active in all hospitals as well as clinics and care homes.. It also has rules for aftercare and appeals.
Your Rights Under the Law: Mental Health Act 1983
If you or someone you know has mental illness, you have following rights under Mental Health Act 1983:
Right to fair care
Your treatment should be designed around your needs. Clear protocols ensure every patient receives fair and consistent support. This helps you feel safe and supported.
Right to be heard
You can share your views on your treatment plan and daily care. Your opinions must be taken seriously, and you can ask for a meeting if you feel ignored. Speaking up helps staff understand what works best for you.
Right to be free from abuse
You should never face harm, bullying, or neglect while in care. If you feel threatened, you can report it to a senior staff member or advocacy service. Keeping you safe is a legal duty for all professionals.

Right to appeal detention
If you are held under the Act, you can challenge that decision in a tribunal. You will be given information on how to apply and who can help you. This process lets you argue your case in front of an independent panel.
HL v UK Case
In HL v UK, a disabled man (HL) was informally held at a hospital without proper legal process. He could not leave and staff made decisions for him. He claimed under Article 5, and the European Court of Human Rights said his right to liberty was breached. This led to changes in the Mental Health Act to include formal safeguards for people who cannot consent to care. Added patient safety checks
Right to privacy and respect
Your personal information and treatment details must stay confidential. Staff knock and wait for your response before they come in. They speak politely and treat you with respect in every interaction to protect your privacy and dignity.
You can use these rights in schools, jobs, homes, and even courts.
Why Mental Health Act 1983 Matters for Healthcare Staff
The Act guarantees fair treatment for patients. It helps reduce stigma and mental health bias in healthcare and law. Patients can:
- Refuse treatment (in some cases), because when you have capacity, you can refuse treatment. Staff must explain the risks and alternatives so you can make an informed choice.
- You can appeal a detention decision through a tribunal if you believe it’s wrong.
- Get aftercare under Section 117. This may include therapy sessions, medication reviews, and help with housing or benefits.
In 2022–23, authorities detained over 51,312 people under this Mental Health Act 1983.
Key Roles of Health Experts under the Mental Health Act 1983
1. Sectioning
- If you’re in a mental health crisis that puts you or others at serious risk, doctors can admit you to hospital without your consent. Two different doctors must examine your situation and agree on the need for detention, each relying on clear medical evidence.
- Detention can cover a short period for assessment or longer for treatment, depending on what the person needs.
2. Patient Rights
If you’re brought into hospital under the Mental Health Act 1983, you do not lose your say in your own care. Staff should sit down with you in plain, everyday language to explain why you’re here and what the next steps will look like. You can speak to a solicitor and ask for an independent mental health advocate to support you. You also have the right to know how long your detention might last and what reviews will take place.
Legal Safeguards
People admitted under the Mental Health Act 1983 can request a review by a Mental Health Tribunal. Panel members study your medical notes and listen to your own account. If they find continued detention unnecessary, they’ll order your release. When the Tribunal grants release, the hospital arranges your discharge. Your social worker or chosen advocate can help you complete the application and prepare for the hearing.
3. Review and Care
A psychiatrist, a nurse and a social worker meet with you at regular intervals. In these meetings they check how you’re doing, update your treatment plan when your needs change and agree on what happens next. As you get better, they put in place follow-up support to help you return to everyday life safely.
Doctors must apply the Mental Health Act 1983 carefully, balancing safety and individual rights.
Mental Health Law for Healthcare Professionals Guide
Doctors, nurses, and mental health staff must know the law. They must give:
- Safe treatment
- Ethical treatment
- Lawful services
This is where the Mental Health Law for Healthcare Professionals Guide helps.
It teaches staff how to:
- Spot abuse
- Report harm
- Follow rules when a person lacks capacity
Staff who ignore these legal requirements could face court action.
Other Legal Tools: The Mental Capacity Act 2005
This Act steps in when someone can’t make their own treatment decisions. Under it, doctors assess a person’s ability to decide for themselves and, if they lack that capacity, make choices in the person’s best interest. In this way, it protects individuals with severe learning or mental impairments.
Read more details about What Is Testamentary Capacity.
Guidelines from Professional Bodies
Apart from the law, other UK groups also guide about treatment:
- GMC: General Medical Council
- NMC: Nursing and Midwifery Council
- HCPC: Health and Care Professions Council
Their rules help health staff act within the law and avoid mental health stigma.
How Mental Health Stigma Affects Lives
Mental health stigma and awareness are two sides of a coin. Stigma is the shame or blame placed on people with mental illness. This can be:
Public stigma
When people hear “mental illness” and think “weak” or “dangerous,” it can shut down any chance of asking for help. Rumors, teasing, or being left out often follow. That isolation makes it even harder to reach out.
Self-stigma
Blaming yourself for your struggles brings shame. You may hide your feelings and skip appointments. Over time, avoiding support only makes recovery tougher.
Legal or institutional bias
Some laws and policies assume mental health issues mean someone can’t be trusted. That bias shows up in child custody cases, court sentences, or when services are denied.
This leads to:
Less care access
Worries about being judged keep many from seeking help. Delayed treatment allows symptoms to grow and become more challenging.
Poor job chances
Employers might doubt a person’s reliability or skills. This can block promotions or even cost them their job.
Bias in legal outcomes
Sometimes a quivering voice or trouble focusing is read as lying or aggression by police or judges. Because of this, someone might get stricter bail conditions, a longer sentence, or lose access to support. A UK Parliament study found people with mental health problems die 15 to 25 years earlier on average than others. It underscores the real cost of these errors.
Impact of Mental Health Stigma on Legal Outcomes
Bias in courts and law can be deadly. People with mental health issues may face:
- Unfair treatment in custody cases, such as Judges viewing them as unstable and removing their children from their care.
- Jurors doubt their testimony, doubting what happened, who was involved, or key details of the incident, assuming confusion.
- Mistaken use of force during arrest for instance police officers mistaking a panic attack for aggression and using excessive force.
Judges, police, and juries may hold hidden biases. This affects the legal outcome even when the law is on the patient’s side.
Fighting Stigma: What Can Be Done
The UK has launched campaigns with charities to challenge misconceptions and reduce mental health stigma by spreading awareness. However, significant gaps remain that demand further action. Here are steps that can help:
Education
- Teach kids about mental health in school.
- Train doctors, teachers, and lawyers on empathy and rights.
- Add courses on mental health stigma and awareness.
Policy Reform
- Review laws to protect against bias
- Improve access to mental health services
- Fund public awareness drives
Community Support
- Promote open talks at work, school, and home
- Help people share their stories
- Challenge the media that spreads false ideas
Better Healthcare Practices
- Train staff on Mental Health Law for Healthcare Professionals Guide.
- Hold team meetings to discuss patient care.
- Make care plans that match the law and patient needs.
The Role of Multidisciplinary Teams
Treatment in the UK is team-based. A care team may include:
- Psychiatrists
They are medical doctors who diagnose mental health conditions and map out your treatment. They may prescribe medications, suggest therapies, and do regular checkups to see your recovery.
- Nurses
Staff check vital signs, administer pills, and watch how patients respond day to day. They deliver your medications on schedule and note how you respond. Any changes get passed along to your doctor right away.
- Social workers
They help you sort out practical needs like housing or benefits applications. They will walk you through any paperwork and help set up that first meeting or call.
- Therapists
Experts provide face to face counseling or group sessions to help patients work through thoughts and feelings.
Each person has a legal role. They must:
- Share updates by sending reports or speaking at team meetings so everyone knows the patient’s progress.
- Review treatment in regular case reviews to decide if medications or therapies need changing.
- Record notes immediately after every contact to keep a clear, lawful record of what happened.
This keeps care safe, fair, and within the law.
Let’s End the Stigma
The Mental Health Act 1983 and other UK laws protect your mental well-being. But we must also fight mental health stigma. This means:
- Knowing your rights
- Getting fair treatment
- Helping others understand
Change begins with awareness. And support begins with care.
Get Legal and Clinical Mental Health Support
Concise Medico provides expert psychiatry witness reports, mental health assessments, and legal-medical opinions aligned with the Mental Health Act 1983. Our team makes sure evaluations follow UK laws. We also promote patient dignity and work to reduce mental health stigma.
Contact Us to learn more or book a consultation.